Dermatomyositis: Everything You Need To Know
Dermatomyositis (DM) is a rare type of autoimmune disease that affects skeletal muscle and skin. It is characterized by the appearance of muscle weakness and a skin rash of a particular nature. According to a publication in the journal Rheumatology, up to 50% of DM cases are associated with the presence of some type of cancer.
The incidence of this disease is estimated to be 4 to 6 cases per million inhabitants. It is a pathology of universal distribution, although it is more common in people of Caucasian ethnicity and in women, who have twice the risk of suffering from it. Are you interested in knowing more about it? Keep reading!
Causes of dermatomyositis
According to the Journal of Clinical Rheumatology, dermatomyositis falls into the group of idiopathic inflammatory myopathies, that is, of unknown origin. Without going into much detail, we will say that these conditions can be divided based on the type of antibodies produced by the sick person.
These antibodies are usually directed at certain enzymes, which participate in the synthesis of proteins necessary for the proper functioning of the body. Dermatomyositis has been associated with the presence of the anti-Mi-2 antibody —among others—, although the underlying autoimmune mechanisms are still under study.
As we have said, the origin of DM is not fully known, but 15% to 50% of cases are associated with cancers of the abdomen, lung and other types of neoplastic tumors, as indicated by the United States National Library of Medicine. . It is also suspected that it may be caused by muscle viral infections and other environmental factors.
It is necessary to emphasize, at this point, that there are 3 types of dermatomyositis. The magazine «Skin. Continuing education in dermatology »explains them as follows:
- Classic DM: when the skin lesions are manifested together with the characteristic muscle weakness.
- Amyopathic DM or AMD: dermatitis is not associated with clinical muscle signs for at least 6 months after the appearance of skin lesions. Despite the symptomatic normality, patients with AMD already show signs that something is wrong with biopsies and muscle ultrasounds.
- Juvenile DM: when these symptoms appear in people under 18 years of age.

Symptoms
As we have said, the symptoms of this disease are cutaneous and muscular, since the antibodies mistakenly attack elements that promote the synthesis and repair of these tissues. According to the Mayo Clinic, clinical signs can appear suddenly or progressively, and are divided into 2 large blocks:
- Skin changes: A characteristic purple skin rash appears, which may appear jointly on the upper eyelids. It also occurs on knuckles, elbows, knees, chest, and back. This rash can be itchy and painful and is the first obvious clinical sign of dermatomyositis.
- Muscle weakness: pain, stiffness, muscle weakness, swallowing problems, and shortness of breath. These signs begin in the muscles closest to the left and right trunk, but progressively spread. Depending on the severity of the condition, this symptom may be disabling.
In turn, these manifestations can be sudden or can appear in a matter of weeks or months. At some point, the patient may have difficulty performing basic tasks such as raising the arms, standing up from a sitting position, or going up and down stairs.
Possible complications
A person with DM has up to 6 times the risk of having some type of cancer. Thus, the most feared complication when making this diagnosis is that the patient has a malignant tumor in the abdomen, lungs or another part of the body.
According to the Myositis Association, 95% of patients survive 5 years after diagnosis. Some of them have a period of acute illness that disappears, while others show symptoms for the rest of their lives.
How is dermatomyositis diagnosed?
The Arthritis Foundation emphasizes that the diagnosis is often difficult and controversial, since in many cases the clinical signs of DM overlap with those of other diseases. In general, the following steps are followed to make a proper diagnosis:
- Medical history and physical examination of the patient.
- Blood test for antibodies and muscle enzymes: The enzyme creatinine kinase (CK) test is often very helpful in diagnosing dermatomyositis. High levels of this organic molecule often coincide with symptomatic peaks.
- Electromyograms: tests that measure electrical patterns at the muscle level.
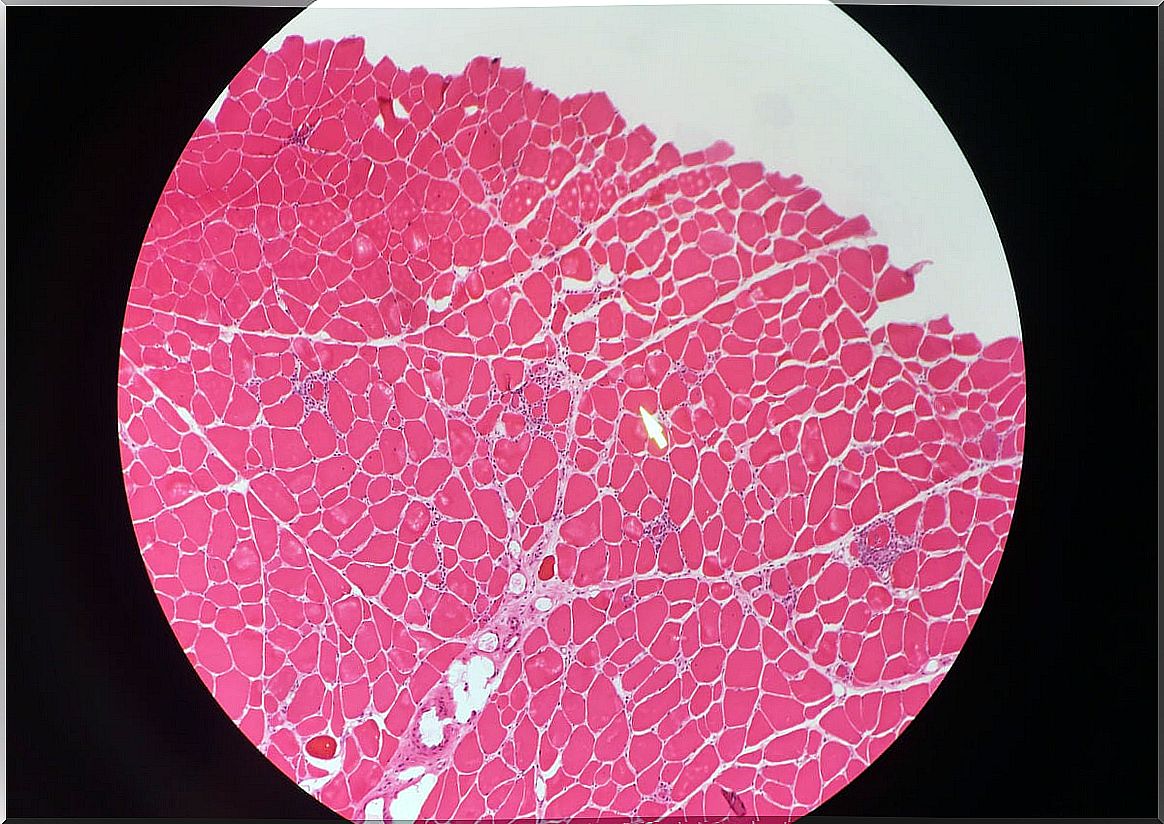
- Muscle biopsy, in order to quantify the damage produced on the tissue.
What are the treatment options?
As it is a low incidence disease, knowledge about the approach and treatment of dermatomyositis is very limited. The central axis of therapy are systemic corticosteroids such as prednisone or cortisone, anti-inflammatory drugs that seek relief of symptoms.
Immunosuppressive drugs – which aim to decrease the action of antibodies – or rheumatoid arthritis drugs may also be prescribed when initial therapies are not effective. All of this must be accompanied by monitored physical therapy and, in some cases, surgeries. The approach is interdisciplinary, as there is no exact solution.
Medical consultation is essential
Dermatomyositis is a very rare disease in the general population and, unfortunately, in many cases it is associated with some type of cancer. The underlying mechanisms that cause the activation of these erratic antibodies are not yet known, so environmental factors such as viruses or toxins, for example, are also being considered.
If you have any type of skin rash, it is most likely not DM, at least statistically speaking. In any case, before any skin rash, go to the doctor promptly, since multiple bacteria and viruses are the cause of this initial clinical sign.