Eosinophilic Fasciitis: Causes And Treatment
Eosinophilic fasciitis is a rare disease characterized by symmetrical inflammation of the extremities. This is usually followed by swelling and induration of the affected areas. It is also known as Shulman’s syndrome.
In other words, patients have a high blood eosinophil count, which is abnormal. However, the peripheral blood eosinophil count is not directly related to the severity of the case.
Eosinophils are granulocyte-type leukocytes. These participate in pro-inflammatory processes, especially in the pathogenesis of allergic diseases. One of its main characteristics are the numerous granules that they present in their cytoplasm.
These granules contain different enzymes, among which histaminase stands out. This is a hydrolytic enzyme that breaks down histamine. Thus, it can regulate the allergic response.
Etiology and pathophysiology

The causes of eosinophilic fasciitis are not known. However, it can be deduced that it is due to an abnormal activity of pro-inflammatory mediators. These alter the thickness of the fascia causing multiple discomforts.
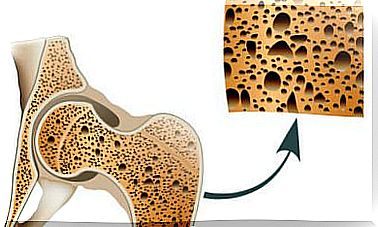
The fascia is a connective tissue structure. This extends like a three-dimensional network and surrounds the internal structures. Thus, it works as a protective mesh due to its extreme resistance.
According to the bibliography, it is observed that a history of extreme sports activity is common in patients diagnosed with this disease.
However, this observation has not provided any conclusive data that can help us understand what triggers eosinophilic fasciitis.
Symptoms of eosinophilic fasciitis
The first signs of the disease are common to those of other inflammatory conditions. These would be pain, swelling, inflammation, and so on. Although in eosinophilic fasciitis a hardening of the skin and subcutaneous tissues is quickly observed.
In addition, a characteristic orange peel is usually present, especially on the palms of the hands. It can also be extended to more visible areas such as the face or neck.
Normally people affected by this inflammatory process see reduced mobility of their limbs due to the development of arthritis.
However, muscle power remains intact. It should be noted that muscle pain may occur. In some cases the appearance of metacarpal tunnel syndrome has been described. However, this is rare.
In addition, eosinophilic fasciitis has another characteristic that allows us to differentiate it from other similar inflammatory diseases. And it is that it does not affect the fingers or toes. This is probably because the fascia is not covering them.
Likewise, due to the characteristics of the disease, they are very frequent:
- Fatigue. This is usually associated with muscle and joint pain.
- The obvious and dramatic weight loss that patients experience. This is due to the reduced mobility that this pathology triggers.
Diagnosis of eosinophilic fasciitis
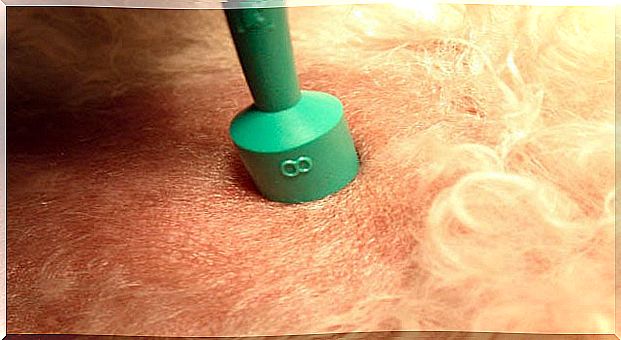
One of the methods commonly used for diagnosis is a complete skin biopsy. In other words, it must reach the fascia and adjacent muscle tissues.
Before performing the biopsy, suspect eosinophilic fasciitis simply by observing typical symptoms. In some cases it can be confused with systemic sclerosis.
Usually it is usually performed an MRI of the extremities. This allows the most altered areas to be observed, which facilitates the selection of the region where the biopsy is to be performed.
Treatment of eosinophilic fasciitis
As it is a disease associated with the overexpression of pro-inflammatory factors and effectors, in most cases it is treated with corticosteroids. The most affected patients may require additional treatment based on stronger immunosuppressants.
In these cases, the most commonly prescribed corticosteroid is prednisone. This is a drug that, after being metabolized, becomes prednisolone, its active form.
In this way it accesses the cell interior. There, it induces the transcription of certain genes. These, in turn, give rise to enzymes related to the arrest of the inflammatory process.
Patients often respond quickly to high-dose prednisone therapy.
However, close monitoring is necessary as it can lead to adrenal suppression. This means that the body is unable to synthesize corticosteroids naturally. Thus, dependency could be generated.