Necrotizing Fasciitis: Everything You Need To Know
What we know as necrotizing fasciitis has other names as well, such as Fournier’s gangrene or gas gangrene . It represents a highly lethal clinical picture that puts the health of those who suffer from it at risk.
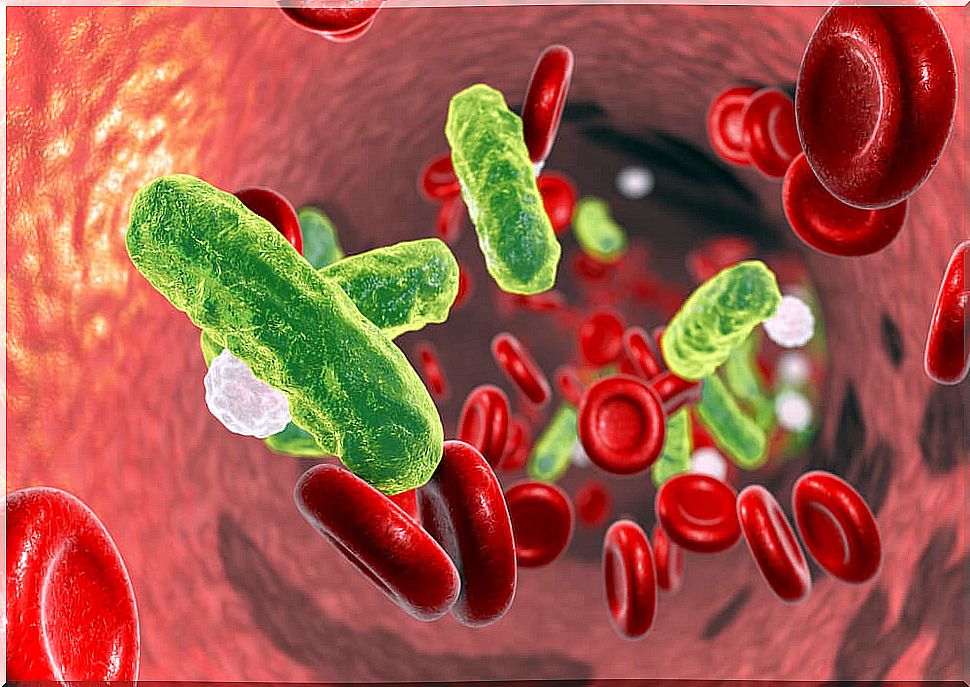
It is a soft tissue infection that kills cells in the skin, the subcutaneous cell layer, and even the muscles. The bacteria that promote this cell death move at great speed and make initial diagnosis difficult.
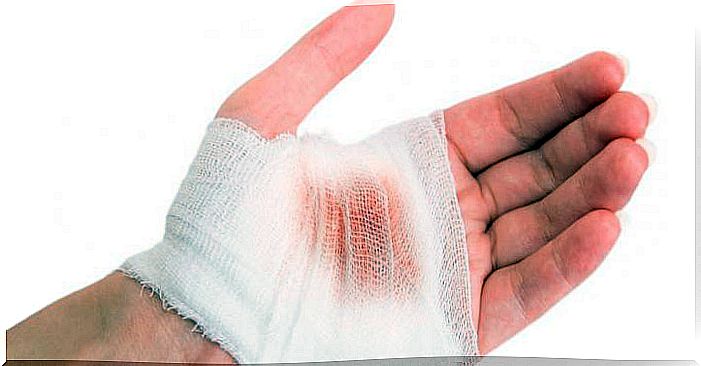
Microorganisms enter the deeper layers of the skin through a small wound or opening. Once inside, they multiply in various ways: some produce toxins and others mobilize the immune system.
Among patients with necrotizing fasciitis who undergo surgery, mortality reaches more than 20%. Mortalities of 40% have been recorded in some series, denoting high fatality.
In children it does not usually appear ; it is considered a rarity in pediatrics. Rather, the risk groups are adults with chronic diseases such as diabetes and cancer.
Symptoms of necrotizing fasciitis
Necrotizing fasciitis progresses quietly at first, which can delay diagnosis and complicate the course and prognosis. The first symptoms do not tend to guide what is happening.
Patients suffer from fever, which can be attributed to other causes when the check-up is done. The pain in the area where the bacteria entered is very powerful, but it does not appear immediately. The painful sign becomes evident when cell death is advanced.
The nerves in that area become inflamed and even infarcted. In autopsies of deceased patients, thrombosis of the small vessels surrounding the necrotizing fasciitis infection has been found.
Sepsis occurs when bacteria or their toxins reach the bloodstream and spread through the body. Once the pathological evolution progresses to sepsis, the symptoms will be those of shock :
- Faintness.
- Loss of consciousness
- Increased heart rate.
- Arterial hypotension
The area of the skin with necrotizing fasciitis also progresses to more complex lesions. Some patients have bruises and other blisters. A classic sign is crepitus, which is the sound that is produced when the region is palpated by the gas that bacteria deposit under the dermal tissue.
The difficulty of diagnosis
When necrotizing fasciitis is detected early, the prognosis improves. However, as we have anticipated, this is difficult at the beginning. During the first 5 days of the disease, the symptoms are nonspecific and the diagnosis is complicated.
In the laboratory there are also no precise indicators. Inflammation parameters such as C-reactive protein and white blood cells increase. A scale, called LRINEC, has been developed that scores biochemical values to improve detection of possible ongoing necrotizing fasciitis.
Once the suspicion has been installed, the doctor requests a blood culture. Through this test, the bacteria that could be colonizing the patient’s blood are grown to find out if they are in the process of sepsis or not.
Imaging studies are not very helpful in diagnosis. Maybe they will do it with the evolution, once the treatment has started, but neither the computed tomography nor the ultrasound are accurate. Both complementary methods are nonspecific and depend on the skill of the operator.
Treatment of necrotizing fasciitis
This disease evolves quickly and the healthcare team must move faster to improve patient survival. Antibiotics and surgery are used to treat necrotizing fasciitis, as well as life support if there is shock.
Antibiotics target the bacteria behind this serious skin infection. Broad spectrum and combination drugs are prescribed to cover several microorganisms at the same time.
The surgical approach is debridement, that is, the opening of the infected area so that oxygen enters and the anaerobic bacteria that live without it die. In the long term, a new plastic and reconstructive surgery will be necessary to close the skin.
If there is shock due to sepsis, the patient will be admitted to intensive care and will receive the protocols of these extreme care. In case of respiratory failure, he will be connected to a respirator; if cardiac arrest occurs, stimulation with drugs will be carried out.
Necrotizing fasciitis is not just a skin disease
In this case, necrotizing fasciitis is not a simple cellulitis or a temporary dermatitis. Even with treatment applied on time, many patients die from the virulence of the infection.
If you have a lesion on the skin that does not heal or that does not progress as it should towards the scar, you should consult your doctor ; much more if it is accompanied by fever and deep pain that you cannot calm.